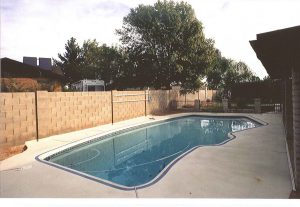
Will Medicare Pay for a Swimming Pool?
Swimming pools offer numerous benefits for individuals, including Medicare beneficiaries. Beyond the refreshing and enjoyable aspect, pools can also provide therapeutic advantages. We’ll explore the potential of Medicare paying for a swimming pool and how pool activities can increase the quality of life for Medicare beneficiaries. Will Medicare pay for a swimming pool? Medicare, in
Better Medicare Alliance
The Better Medicare Alliance is a research group in the United States that supports private health insurance coverage for Medicare recipients through Medicare Advantage plans. Aetna, Humana, and fund the 501©(4) group. Please continue to read below and learn more about the Better Medicare Alliance’s work. Better Medicare Alliance: Who are they? The Better Medicare
Best States to Retire (2023)
Choosing the right state for retirement is a crucial decision that can significantly impact your quality of life, finances, and healthcare access. To help you make an informed choice, this article will explore the best states to retire in 2023, considering factors like cost of living, healthcare facilities, climate, and cultural amenities. Factors to consider
Medicare’s What’s Covered App
Navigating Medicare coverage can be complex, but with the new Medicare What’s Covered App, understanding your benefits has never been easier. As a Medicare beneficiary, you deserve convenient access to comprehensive information at your fingertips. This article will explore the What’s Covered App’s features, benefits, and practicality, ensuring you can confidently make informed healthcare decisions.
Best Health Insurance Options for Seniors and Retirees in 2023
Good health insurance is crucial for keeping good health and handling healthcare costs as you retire. We’ll explore the top 10 best health insurance options for seniors and retirees. These plans offer complete coverage and cater to the unique needs of individuals like you. Importance of health insurance for retirees and seniors Health insurance plays
Medicare Freebies – What You Need to Know
When you join Medicare, you’ll soon learn all the fantastic perks of this popular health insurance coverage. But are you aware of the extra, extra perks? Such as program freebies? Below we’ll uncover the benefits often included with Medicare that are lesser-known among beneficiaries. While Medicare isn’t exactly free, since you pay Medicare expenses such
Guide to Library Programs for Seniors
Are you a senior looking for activities to stay engaged and active in your community? Libraries offer various resources and programs, from books and magazines to art classes, lectures, computer training—and much more. This guide will explore different library resources geared specifically toward seniors and provide tips on finding the right program suited to their
The Top 5 Tips for Long-Distance Grandparenting
Being a grandparent is a special role, but staying connected and involved in their lives can be challenging when you live far away from your grandkids. However, with the help of technology and a little creativity, long-distance grandparenting can still be a fulfilling and rewarding experience. In this blog post, we’ll share the top 5
Senior Voting: Why It Matters and How to Overcome Barriers
As the fastest-growing demographic group in the United States, senior citizens significantly impact the outcomes of elections. However, many seniors face barriers when exercising their right to vote. This post will discuss why senior voting matters, common obstacles seniors face, and tips for overcoming those barriers. Why senior voting matters: Power of the senior vote
Breaking the Stereotypes: Overcoming Ageism in Today’s Society
As we grow older, we often face many challenges in our daily lives, one of which is ageism. Ageism refers to discrimination against individuals based on their age, and it is unfortunately all too common in our society. For Americans over the age of 63, it can manifest itself in many different ways. Consequently, there